‘Ealing in the 1918-19 Flu pandemic’ by Dr Peter Hounsell. Chair of Ealing Branch HA
It was predictable that in the midst of the 2020 coronavirus pandemic, that epidemiologists and historians should look back to the influenza pandemic that ravaged much of the world in 1918-19, and which was in any case fresh in the mind as its centenary had only occurred a couple of years earlier. It is hoped that the 2020 event will be, like its predecessor, a once in a lifetime, or once in a century, event. Despite two world wars, and several acts of genocide, the flu pandemic of 1918-19 remained the worst demographic disaster of the twentieth century with an estimated 30 million deaths worldwide, and the most devastating infection to strike the world since the Black Death, five hundred and fifty years before.
It seems to have started in one place and spread worldwide, leaving only a few isolated island communities unaffected. The virus was a new strain of influenza to which there was little natural immunity, and was accompanied by high levels of morbidity and mortality. The symptoms of the disease were severe headaches, body pains and fever, not inconsistent with other forms of flu, but in severe cases it led to pneumonia and cyanosis. An attack usually lasted for two to three days, but could become deadly once bacteria entered the lungs. The onset of the disease could be sudden, with reports of people collapsing in the street, and dying within a few hours.
Doctors, even in countries with well-organized medical systems, had little therapeutic means at their disposal to deal with the outbreak. This wasn’t because they hadn’t encountered influenza before. There had been epidemics of flu since the 1830s, and the Registrar General had been recording deaths from influenza from 1837. Many people in positions of authority in 1918 would have remembered a serious outbreak in 1889-90, which had been known as ‘Russian Flu’. Seasonal flu, then as now, was something people lived with, and some people died of, every year.
The pandemic of 1918-19 was different, for a number of reasons. Seasonal flu usually arrived in the winter months and faded away in the warmer conditions of spring and summer. The pandemic first showed itself in Europe in late spring/early summer. Despite the name given to it at the time ‘Spanish Flu’, later research – and historians continue to research the origins of the disease – indicates that this strain of flu did not originate in Spain. The reason why the term ‘Spanish’ became attached to this particular strain seems to be related to the wartime conditions of censorship. Spain as a non-combatant nation in the First world war, had an uncensored press, unlike most of its European neighbours, and reported the high incidence of infection in the country – including its king. The French and British authorities, by contrast, did not want to let their civilian population, or the enemy, know the impact flu was having on the fighting capacity of its armies, although the British press were able to report on the effects on the German army and on its cities.
Modern research suggests that this new strain of flu had one of three possible origins. The first was an outbreak in China in 1917-18, which was spread by recruits in the Chinese Labour Corps on their way to support the allied war effort on the Western front, some of whom took the easterly route across Canada; the second was the outbreak of what medical doctors at the time termed purulent bronchitis which had affected British soldiers who had been gassed and were being treated at the huge army base at Etaples in the autumn of 1916; the third, that it started in a rural community in Kansas, from which recruits to the US army were taken. In this case it may an example of a disease that jumps the species barrier, from wild birds to humans. The nearby Fort Funton, which recruited from the surrounding farming communities, experienced an outbreak in March 1918. The US government, having entered the war, was now sending large contingents of soldiers to the Western Front, and from the United States troopships spread the virus rapidly in March and April to Europe, then to Asia and North Africa, reaching Australia by July.
Since the micro-organism responsible for this strain was not identified until 1933, unlike the coronavirus which was genetically sequenced very quickly after its appearance, there was no reliable test available to doctors at the time. They would have been familiar with general influenza systems, and initially reacted in tried and trusted ways, but this disease proved far more difficult to manage.
The war almost certainly played a large part in the rapid transmission of the virus from its point of origin across the world. In 2020 it is air travel that facilitates the movement of the virus across continents, in 1918 it was troop movements, and particularly the large-scale transfer of men across the Atlantic to the battlefields of Belgium and northern France. Many people were affected by that first wave of the disease in the spring and early summer of 1918, but it did not seem very deadly, and with the war not yet won (in hindsight we can see that by the summer of 1918 the tide was turning in favour of the allies, but for contemporaries this would not have been apparent) there was an urgent need for the troops to be returned to the front line, and the workers back home in industries like munitions to keep producing the materiel of war.
However, there was a second wave. The virus seems to have mutated and a much deadlier strain began to circulate in the autumn of the 1918. By September the flu had spread throughout much of Europe, killing 100,000s of people, and leaving even well-equipped medical services struggling to cope. There was a third wave in the spring of 1919, but with much decreased virulence and many fewer deaths. The war ended, of course, in the midst of the second wave, causing further potential for the spread of the disease as soldiers were demobilized and returned home.
All the combatant nations were hit hard: in Britain mortality exceeded 200,000, slightly more in France, and over 250,000 in Germany. There were over 650,000 deaths in the USA.
So, what was the experience of people in Britain, in London, and specifically in Ealing?
People in Britain would have become aware of the disease at the beginning of June when newspapers began to run stories, especially picking up the news coming out of Spain about a ‘mysterious new disease’ which was affecting up to 8 million people (some 40% of the population) and paralysing the life of the nation. At the same time the disease was prevalent in Sweden.[1] A few days later Belfast was in the grip of an influenza like disease, then Berlin. [2]
Outbreaks in continental Europe may been concerning, but it was the arrival of the disease in England on 19 June that worried the medical authorities. Wounded soldiers, evacuated back to England, and recovering in the King George Hospital in Southwark, appear to have brought the disease with them. A couple of days later attacks of the disease were being reported in several parts of London, with people collapsing in the street. However, despite the sudden nature of its onset, many sufferers experienced the usual flu-like symptom of a high temperature and headaches, and were advised to take to their beds until they felt better.[3]
Even if the disease did not seem severe, the number of cases occurring in London, and elsewhere in the country, began to have an impact on daily life. City businesses were affected by staff absences, and there was a run on pharmacies for a range of medicines that were said to offer protection. A Fulham chemist suggested Dr Broughton’s fever mixture (which was a mixture of quinine, cinnamon and eucalyptus amongst other things) was a ‘certain preventative and cure’ for the sum of 1s 3d. At this point there were many absences in schools, but there had not been a call to close them.[4]
Things began to turn darker when the first deaths attributed to the disease were reported. Two boys both 10 years old had died, one said to be definitively of the disease and another with a strong presumption that this was the cause. In another case a 13 year old pupil of a convent school had been taken suddenly ill and died the following day. A further 62 children at the same school were also ill.[5] A few days later a young mother who had earlier been playing cricket with her children complained of the loss of power in her legs, then became unconscious and died.[6] At one of the inquests, the coroner, asked that the windows be open, arguing that ‘a little draft is better than infection’[7]
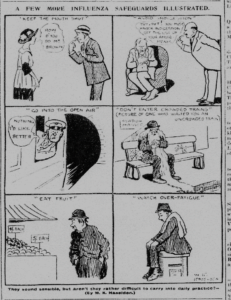 At this point advice began to be offered about how to avoid catching the disease. In cartoon form the Daily Mirror advised people to ‘keep the mouth shut’, ‘avoid indigestion’, ‘go into the open air’, ‘don’t enter crowded trains’, ‘eat fruit’ and avoid ‘fatigue’. [8] You perhaps need to be reminded that at this point in the war food rationing was in force. One enterprising Harrow grocer even suggested a well-nourished body was the answer, and one of the best sources of nutrition was the real Turtle soup that his shop could supply.[9]
At this point advice began to be offered about how to avoid catching the disease. In cartoon form the Daily Mirror advised people to ‘keep the mouth shut’, ‘avoid indigestion’, ‘go into the open air’, ‘don’t enter crowded trains’, ‘eat fruit’ and avoid ‘fatigue’. [8] You perhaps need to be reminded that at this point in the war food rationing was in force. One enterprising Harrow grocer even suggested a well-nourished body was the answer, and one of the best sources of nutrition was the real Turtle soup that his shop could supply.[9]
There were examples of concerts and other events being cancelled because the participants were ill. The outbreak was, is was said, playing havoc with the casts of some theatres and music halls, which meant that deputies and understudies were in great demand. [10]
Ealing and Acton were not immune from the disease. The Acton Medical Officer estimated there were 1,000 cases in early July of which he had personally seen about a hundred. On 6 July there were said to be many cases in Ealing and 50 people employed by Ottways, a firm which made optical equipment particularly for the military, were off sick on a single day.[11] A couple of weeks later 1,000 Ealing schoolchildren were absent along with many of their teachers.[12] But by then there were signs that the epidemic in London was slowing down, whilst numbers were still high in the provinces. [13]
In 1918 there was nothing like the modern National Health Service. Each town or borough had its own Medical Officer of Health, not always a full-time job, but these were medically trained, and had broad responsibilities for the public health, ranging across the regulation of food traders, sanitation, and the control of infectious diseases. They were used to seasonal flu, as well as dealing with dangerous illnesses such as diphtheria, measles and tuberculosis. Importantly, for controlling this outbreak, influenza was not a notifiable disease, that is you did not need to report to the authorities if you thought you had it. There were some general hospitals, and there were infirmaries attached to the workhouse, as well as isolation hospitals for people with contagious diseases. There was no Ministry of Health, although it was already being planned, and would come into force at the end of the war. Action was taken on a local level and co-ordination of the response to the epidemic was the responsibility of the Local Government Board, which supervised local government, and had its own Medical Officer.
The authorities had limited resources to respond to an outbreak like this, especially as the disease was little understood. So, the advice given by the LGB relied heavily on personal responsibility. Sir Arthur Newsholme, the Chief Medical Officer of the London County Council and the Chief Medical Adviser to the LGB (the Chris Whitty of his day) had this to say
‘Epidemic influenza is a disease the spread of which cannot be controlled by the action of the public authorities. It is extremely infectious and the incubation period being a question of hours or only two or three days, cases multiply with lightning rapidity. The symptoms vary from those of ordinary catarrh to a disease of much severity. When there are only catarrhal symptoms without much constitutional disturbance patients continue work and thus disseminate the disease broadcast. It is desirable to avoid persons suffering from bad colds, especially persons seen to be using handkerchiefs or sneezing. There is little doubt that over-fatigue and a dry dusty atmosphere favour infection. Persons beyond middle life should take special precautions to avoid crowded assemblies and other places where infection is likely to be prevalent. An approximation to open air conditions (doors and windows open) even when in the house or office, is one of the best means to diminish the risk of infection.’[14]
Towards the end of July the outbreak subsided. As the Ealing Medical Officer, Dr Orr, noted, it was difficult to put an accurate figure on the number of cases, since it was not a notifiable disease, but an idea of the prevalence came from school attendance figures. The disease had been of ‘a mild character’ with the children recovering quickly, but adults had also been affected, but it was his opinion that the infection had been spread by the schools. In this outbreak they had been few deaths, none in June, but six in July, although none of the them had been children.[15]
With few cases of influenza during August and September there might have some confidence that the disease had been seen off. Sadly, this was not to be the case, and the disease returned with greater virulence in the autumn and winter. It is possible that the virus may have mutated, but the medical researchers of the time did not have the tools to investigate this. By late October the country was in the grip of a second wave. In Ealing hundreds of people were taken ill, with the south west of the borough the first to feel the impact of the disease. The Medical Officer started to close schools to control the outbreak, starting with Northfields School. Then it became necessary to close all schools for 10 days to try and control transmission. At this point across the borough 35% of children were already absent. [16] I
The local paper reported the early deaths – a teacher who had taught at Lammas School, a lady assistant from a draper’s shop.[17] The advice being given to the local population remained much the same as it had been during the early summer: avoid scattering infection by coughing and sneezing, always carry a handkerchief, clean the homes and bed linen of people who had been affected, ventilate rooms, and avoid overcrowded places such as places of entertainment. It was realized that some people were at greater risk of being taken seriously ill, and developing pneumonia, and immoderate drinkers were singled out. People with existing medical conditions and the elderly would need to be protected.
Stress was laid on the need to act responsibility, and to avoid transmitting the disease to other people.
If every person who is suffering from influenza or a cold recognized that he is a likely source of infection to others, that some of the persons infected by him may die as a result of this infection, and took all possible precautions, the present disability and mortality of catarrhal epidemics would be materially reduced.[18]
Dr Orr was to be disappointed by the public response. Reflecting on what had happened in his annual report he condemned the failure of the public to take steps to prevent the spread of the disease; they had acted ‘with a disinterestedness, or even it might be said, a callousness, which brought disaster to many families’. A harsh judgement indeed.[19]
It is was at this time that there was a focus on the danger posed by people crowding into cinemas. With schools shut there was a danger that children would spend time in cinemas. The medical officer and his assistants visited Ealing’s four cinemas and asked them to exclude children from performances, but met with some resistance. Eventually in early November the Middlesex County Council (the licensing authority for cinemas) issued new regulations, specifying that during periods of epidemic disease no children under the age of 14 should be admitted to a cinema. The new regulations stopped continuous performances, so that the cinema could be emptied, cleaned and ventilated between showings.[20]
November marked the peak of the second wave of the epidemic. Doctors were being worked off their feet treating cases, and there were many deaths. The week ending 11 November was the worst week of all with 37 deaths, and there were 87 in the whole month. This naturally put a great strain on undertakers and the cemetery. One Ealing undertaker had taken 20 orders for funerals in a week, and complained that he had insufficient men for the work involved. ‘We have been working day and night, and four or five bodies which ought to have been in coffins on Wednesday will have to wait until Saturday. The state of affairs in unprecedented’. It was the same at the cemetery: the gravediggers had been unable to cope with increasing demands, and soldiers and other council workers had been called in to help out. On one day there had been 18 funerals at Ealing cemetery.[21]
The number of deaths went down steadily during December and the epidemic seemed to dying down. As winter gave way to spring, it might have been hoped that the Spanish Flu, like seasonal influenza, would fade away until the autumn, but this disease played to different rules, and there was to be a third wave. The local paper alerted its readers at the beginning of March that influenza was spreading again, and there had been 16 deaths in a week. Fortunately, this third outbreak was short-lived, and from the beginning of April it ceased to be newsworthy.
A number of factors had contributed to the spread of the disease and the difficulties on dealing with it, as Medical Officers of Health across the country commented in their annual reports. They regretted they had little resources to deploy in the face of an outbreak of this kind, and although there was a good understanding of the challenges of seasonal flu, this disease was highly virulent and deadly. It had another unusual characteristic. The groups in the community most at risk traditionally from seasonal flu are children, and the elderly. This epidemic had a marked impact on what were usually the least vulnerable, young adults. Over the three outbreaks 233 Ealing residents had died, of which 27% were aged between 25 and 35. For those between age 5 and 35 females had a much higher death rate than males in 1918 but the position was reversed in the third wave.[22] This gender divide may not tell us much about the disease, it may reflect the imbalance in the borough’s population. In the 1911 census 58% of the population were female, and this rose to 60% of those aged 20-40. Ealing, as a middle class area, had a large number of domestic servants, and 6,590 women gave their occupation as domestic servant in 1911. That gender imbalance presumably widened during the war years when many of the men were serving in the armed forces, and would have affected the death rate in 1918. By the time of the last outbreak in the spring of 1919 many of them would have been demobilised.
There was a shortage of medical staff. It is important to remember that the epidemic hit before the war ended – the armistice occurred at the peak of the second wave. Many doctors and experienced nurses were treating the wounded in military hospitals abroad and at home, and the only resources the local Medical Officers could deploy were health visitors, who could visit homes and give advice, and help nurse serious cases. Many of the doctors who were still working on the Home Front would have been older. People who were seriously ill were admitted to the infirmary of the workhouse in Isleworth, but there was little treatment that could be provided except general nursing. Many of those who became seriously ill died of pneumonia, a not uncommon outcome with all forms of influenza.
The flu pandemic occurred at the end of four years of war, and this had put a great strain on society. Many families had lost loved ones, a great many young men were absent serving abroad, and others, including many women, found themselves working in different occupations to help the war effort. After a period of erratic food supplies, rationing had finally been brought in at the beginning of 1918. Dr Orr remarked that
The severe mental and physical strain resulting from four anxious years of war accompanied by restrictions in diet probably rendered the community more susceptible to infection and more liable to complications when attacked.
Ealing had got off lightly compared to other places. In 1918 there were 880 deaths from all causes in Ealing, so the 158 deaths from influenza were 18% of the total, and equated to 2.5 deaths per 1000 population. In 1919 there were a further 75 deaths out of a total of 802 overall, only 9% of the total. In 1920 there were just 28 deaths from influenza, and the number of deaths was 673. There had been 672 deaths in 1914, so for 1918 the number of excess deaths was around the 200 mark. [23]
The Medical Officer for the London County Council (Ealing was not in the London County at this time) reported a total of 16,520 deaths over the three outbreaks – 989 in the first, 11898 in the second, and 3633 in the third. Some boroughs in London had high numbers of deaths: Poplar had 524 deaths, Lambeth 819, and Islington had 931 (average deaths in this borough from 1908 to 1917 were 48).[24]
Further reading:
An accessible modern account of the influenza epidemic can be found in Laura Spinney’s book, Pale Rider: the Spanish Flu of 1918 and now it changed the world published in 2017.
A more academic study is H. Phillips and D. Killingray (ed.) The Spanish influenza pandemic of 1918-19: new perspectives published in 2003.
In writing this article, the Medical Officers’ reports for London boroughs were accessed online at London’s Pulse, hosted by the Wellcome Library. www.welcomelibrary.org This is free to use.
Newspapers were accessed online via the British Newspaper Archive. www.britishnewspaperarchive.co.uk (subscription required)
Abbreviations used in the notes.
MCT Middlesex County Times; MOH Medical Officer of Health
[1] People 2 June 1918
[2] Globe 11 June 1918; Daily Mirror 17 June 1918
[3] Westminster Gazette 19 June 1918; Globe 21 June 1918.
[4] Pall Mall Gazette 1 July 1918; Fulham Chronicle 5 July 1918
[5] Pall Mall Gazette 1 July 1918; 2 July 1918
[6] Ill Police News 5 July 1918
[7] Globe 3 July 1918
[8] Daily Mirror 3 July 1918
[9] Harrow Observer 5 July 1918
[10] Pall Mall Gazette 6 July 1918
[11] Acton Gazette 5 July 1918; MCT 6 July 1918
[12] MCT 17 July 1918
[13] Daily Mirror 15 July 1918
[14] Pall Mall Gazette 6 July 1918
[15] MOH Report for Ealing 1918, p.15
[16] MOH report p.15
[17] MCT 26 Oct 1918
[18] MCT 26 Oct 1918
[19] MOH Report for Ealing 1918
[20] MCT 9 Nov 1918
[21] ibid
[22] MOH reports for Ealing, 1918 and 1919
[23] Ibid; the MOH reports for 1915-1917 are not in the London’s Pulse collection
[24] MOH report for the County of London; individual borough Medical Officer annual reports
